Abstract
Background: Patients with Chronic Lymphocytic Leukemia (CLL) are susceptible to infections due to impaired humoral immunity, both as a complication of the disease and treatments received. Herpes zoster (HZ) is painful, vesicular rash due to the reactivation of latent varicella zoster virus that is more common in patients with compromised immunity. Fludarabine is a purine analog that has long been incorporated in chemotherapy regimens for CLL and has been known to cause lymphocyte depletion and increased risk of viral infection and reactivation. Bendamustine is a newer therapy that has been increasingly used for the treatment of CLL. The aim of this study is to explore the rates of herpes zoster infection in patients treated with bendamustine compared to fludarabine using the Veterans Administration Central Cancer Registry (VACCR).
Methods: We used the VACCR to identify patients diagnosed with CLL between September 1999 and October 2015. Pharmacy Benefits Management (PBM) records were used identify patients who received bendamustine or fludarabine as initial treatment of CLL. ICD-9 codes for HZ infection (053) were used to identify potential cases. PBM records were collected for prescriptions of acyclovir or valacyclovir at a dose of 1500mg/day or higher within 30 days of ICD9 code and treatment was verified as appropriate for HZ. Comparisons between groups were performed with independent samples t-test or chi-square as appropriate. Comorbidity was assessed with Charlson (Romano) index and outcomes by the Kaplan-Meier method. Cox proportional hazards regression modeling was used to assess associations between treatment while controlling for age at treatment and comorbidity index. The study was approved the Saint Louis VA Medical Center institutional review board.
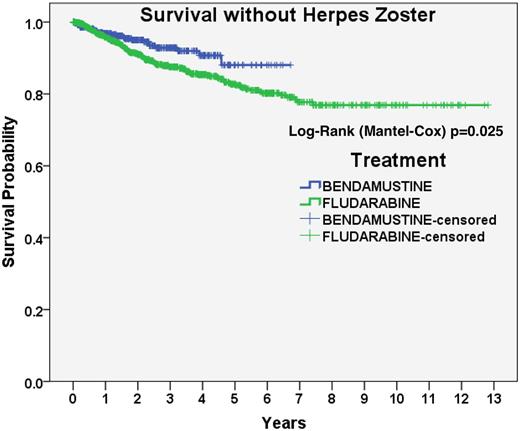
Results: A cohort of 7155 patients were identified and fludarabine was given as initial therapy in 1084 patients and bendamustine in 460 patients. Comorbidities were higher in patients receiving bendamustine compared to fludarabine, (2.11 vs. 1.63, p<0.001) and median age at treatment of patients receiving bendamustine was higher than fludarabine (68.1 years vs. 64.4, p<0.001). Median follow up was 42.8 and 23.6 months for the fludarabine and bendamustine groups, respectively (p<0.001). In univariate analyses, bendamustine was associated with reduced rate of HZ (Hazard Ratio (HR) 0.61, 95% CI: 0.40-0.94, p=0.026). When adjusting for age and comorbidity, bendamustine was continued to be associated with reduced rates of HZ (adjusted HR (aHR) 0.60, 95% CI:0.39-0.93, p=0.022). Five patients (20%) in the bendamustine group and 43 patients (32%) in the fludarabine group had prescriptions for acyclovir or valacyclovir in the year prior to HZ diagnosis (p=0.243).
Conclusions: In this retrospective analysis of CLL treatments, bendamustine was associated with lower rates of herpes zoster compared to fludarabine, even in older patients with more comorbidities.
Sanfilippo: Bristol Meyers Squibb: Speakers Bureau. Carson: Seattle Genetics: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal